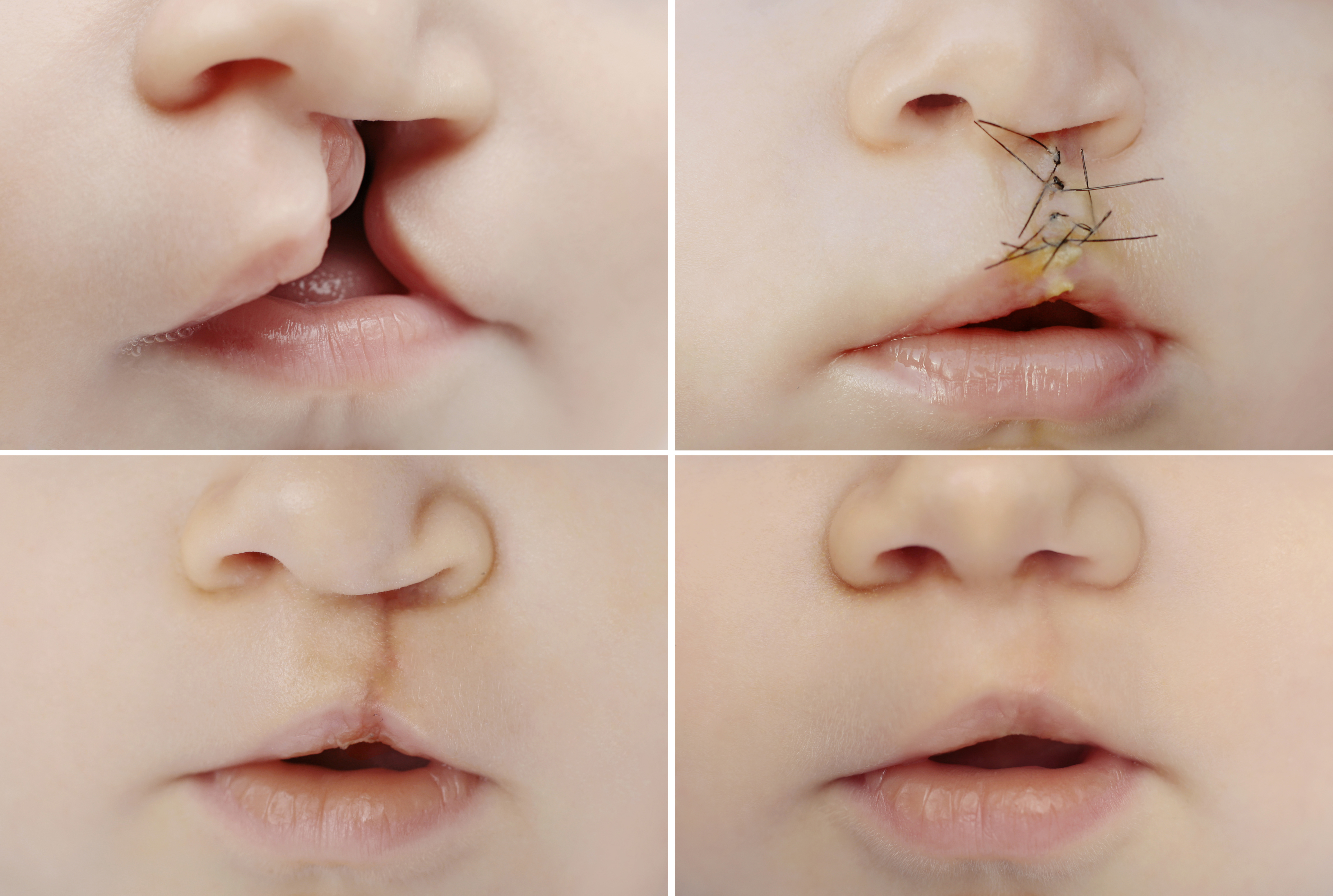
Cleft Lip & Palate Repair
If your child was born with a cleft lip and/or cleft palate. This can be a very upsetting time filled with many questions and concerns. It is normal to be anxious during this initial phase of learning about clefts and the care that they require.
A normal palate extends from the gum line all the way back to the uvula. It separates the oral cavity from the nasal cavity and has three layers. There is an oral mucosa layer, a middle bone layer in the hard palate, or a muscle layer in the soft palate, and there is a nasal mucosa layer. The hard palate does not move, but the soft palate moves and serves a very important function. Elevating against the back of the throat the soft palate closes off the nose and prevents food or speech sounds from coming through the nose. With a cleft palate, not only is there a defect in the palate allowing a connection between the nose and the mouth, but the soft palate is also short, and the muscles are malpositioned leading to potential problems with palate function even after the cleft is repaired. The goals of the surgery are to close the cleft, generally in two layers for the hard palate and two or three layers for the soft palate separating the nasal cavity from the oral cavity.
Some surgeons will attempt techniques to lengthen the soft palate and/or realign the muscles. There is some controversy over which repair technique provides the best results. It is important to understand also that any surgery on a growing infant’s face has the potential to disrupt growth. The desire to repair or close the cleft early has to be balanced with the potential disturbance in the growth of the palate, gums, and middle portion of the face.
Common Questions about Cleft
What is a cleft?
A cleft is simply a hole, or a space in the lip and/or palate where there should normally be tissue. Early in the embryonic period, the tissue did not come together in the region of the cleft, leaving this space.
What causes a cleft?
There are many different causes for clefts. Sometimes the specific cause of a cleft can be identified. However, the majority of clefts are caused by a combination of genetic inheritance and environmental factors. It is generally not something that the parents have any control over. A geneticist or genetics counselor can help you determine if there is a known cause for the clefting and help you determine what the chances are of having further children with clefts.
What challenges will be faced?
There are many challenges that the parents of a child with a cleft and the health care providers will face. Some children born with cleft palate have a small jaw as well which can lead to breathing problems. However, the earliest of these problems is likely to be with feeding. A cleft in the lip may prevent the lips from coming together and pursing for latching on or nippling. A cleft of the palate may prevent the baby from generating negative pressure in the mouth to create suction to deliver milk into the mouth. Breastfeeding may be difficult or impossible for a child with a cleft, however the breast milk can be pumped and delivered with a special feeder. Numerous nursers have been developed to assist in the feeding of a child with a cleft. Different styles of nurser work better for different individuals, but they all have as their purpose the increase in milk flow to the baby’s mouth.
Once the baby is feeding well, growing and gaining weight, surgery to repair the cleft can be planned.
The initial repair of the lip and/or palate is usually completed in most surgeon’s hands by about 18 months of age. Factors such as other medical conditions or birth defects may influence this timing. The type and severity of the cleft will determine the number of procedures necessary during that period. Because children with cleft palate also have an increased incidence of fluid in the middle ear and ear infections, it may be recommended that tubes be placed in the ear drums during one of the cleft repair procedures. In children with cleft palate speech may also be a problem, and speech therapy may be initiated quite early. Even when palate surgery is successful in closing the cleft, the shortness or lack of movement of the palate may result in abnormally nasal sounding speech. Other operations are designed to correct this type of problem should it develop.
The abnormal appearance of the nose associated with a cleft lip usually improves significantly when the lip is repaired. However, further nasal surgery is typically required to improve the symmetry and appearance of the nose. The timing of nasal procedures is based on the severity of the deformity and the surgeon’s preference relative to the overall cleft care plan.
If the cleft passes through the gum line then a bone graft to the gum may be required to allow for proper alignment of the adult teeth by an orthodontist. This is usually done later in the course of cleft care.
As you are beginning to see, care for clefts can be quite complex, requiring the specialized skills of numerous providers. The care tends to proceed most efficiently and effectively if these providers are coordinated and working together as a team. This coordinated, skilled care can lead to happy, fulfilled lives for most children born with clefts.
Understanding the Surgery
The normal lip has three layers, a mucous membrane inside the mouth, a middle muscle layer and an outer skin layer. The skin layer of the upper lip has some anatomic details which the human eye expects to see and notices quickly if they are distorted or abnormal. The line that separates the vermilion part of the lip from the rest of the lip skin is referred to as “Cupid’s bow.” It has a central low point and two flanking high points which make the handle of the bow. The rest of the bow extends to the corners of the mouth. Two ridges or philtral columns typically pass from the peaks of Cupid’s bow up toward the middle portion of the nose.
Not only must the three layers of the lip be reconstructed, but the anatomical details of Cupid’s bow must also be established. The philtral ridge on the cleft side is shorter than the one on the non-cleft side and must be lengthened through one of various methods. Because scarring will be the inevitable result of the lip repair, another goal is to minimize the visibility of the scarring so that the repaired lip can look as natural as possible. In a child with a bilateral cleft lip, the goals are the same but the techniques are frequently modified because of the different anatomy. Two philtral ridges must be established, and the central portion of the lip must be elongated.
What To Expect After Surgery
Cleft lip repair typically takes from one to three hours. Depending on the extent of the surgery and the age and condition of the child, the procedure can be performed on an outpatient basis or may require an overnight stay in the hospital. Many surgeons will recommend arm splints and special feeding techniques, such as syringe feeds, to avoid trauma to the lip. Often the lip will be dressed with a piece of adhesive tape to take the stress off of the sutures, and you may be instructed to keep ointment on the suture line.
Pain medication and antibiotics may be prescribed as well, and you will be given a follow-up appointment so sutures can be removed as needed and that the result of the repair and the healing can be evaluated. Infants tend to heal with fairly pink stiff scars which, with time, will fade and soften, becoming much less noticeable. It is important to avoid any sun exposure to the scar initially as this may permanently darken the scar. The appearance of the nose typically improves significantly after lip repair, and often surgeons will perform minor surgery on the nose during lip repair to further improve its appearance. Minor lip scar revisions are not uncommon to “fine tune” the lip appearance.
Palate repair is typically performed at an older age than lip repair, and it is usually a slightly more involved procedure, generally lasting in the two to four hour range. Most children will stay in the hospital from one to four nights after the surgery. The needs for pain medication are greater, and they have more difficulty feeding. The patient is generally kept on a liquid diet for a week or two after the surgery administered either via a syringe or a “sippy” cup to protect the palate. Arm splints may be required to keep the hands out of the mouth. The follow-up appointment will be set up to evaluate the success of the surgery. Occasionally, a palate repair may not be 100% successful leading to a smaller connection between the nose and the mouth called a fistula. These often shrink and may close on their own, but occasionally, they require a separate surgical procedure to close them.
As the potential for cleft related problems does not end with the successful repair of the cleft, it is critical to continue long-term follow-up with your cleft care provider so that any problems developing with hearing, speech, dental occlusion, facial growth or appearance can be caught early and dealt with appropriately. Because of issues with facial growth, some definitive corrective procedures for the nose and facial bones are best deferred to the teen years.
This is an overview of the long-term care plan which may be needed to fully address the problems associated with clefting. Your cleft care provider can provide you with more information, including support groups of people sharing similar experiences with you.